Manipulating the microbiome with more efficacy and making dietary therapy even more personalized
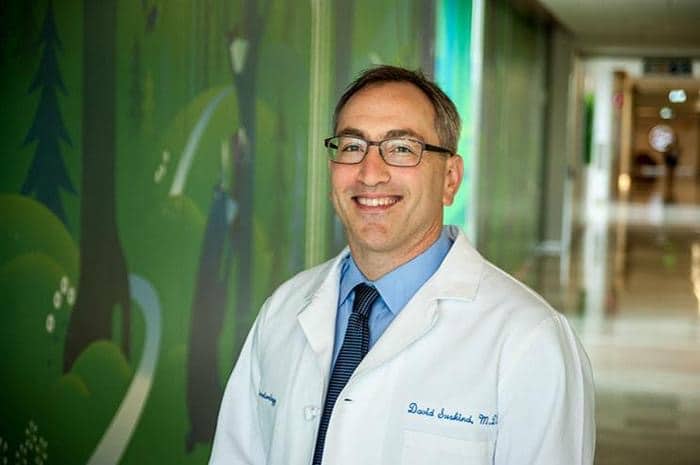
An interview with Dr. David Suskind.
David Suskind is a renowned and accomplished physician. He is a professor of pediatrics and director of Clinical Gastroenterology at Seattle Children’s Hospital. His pioneering research is unraveling the intricate connections between IBD, nutrition, and the microbiome, proving that diet, either as an adjunct or primary therapy, has a profound influence on the microbiome and disease activity.
He is also known as a compassionate and exceptionally skilled clinician who puts patient care above all else. Every summer he volunteers as a camp physician at the CCFA Camp Oasis for young IBD patients, and several times a year he joins his patients at SCD cooking classes for fun informal activities.
Through his research and interaction with patients, Dr. Suskind realized that while diet is a powerful medical tool, it can be very difficult to practice. This led to one of his main goals – making dietary therapy easy to understand and to follow.
In 2015 he published the book Nutrition in Immune Balance (NIMBAL) Therapy . The book is a practical guide for patients and their families, and copies of the book were sent to every pediatric gastroenterologist in the United States.
He also created the site Nimbal, to help healthcare providers and patients integrate dietary therapy as treatment for Inflammatory Bowel Disease. The site includes helpful videos, basic guidelines and practical advice to help navigate the challenges of dietary therapy, and is commonly used as reference when new patients embark on the diet.
What are the odds that a highly regarded professor of medicine will take time to write an entertaining multi-lingual comic book?
In efforts to educate young patients around the world Dr. Suskind wrote a comic book Professor Nimbal: Explorations in Crohn’s and Colitis, to teach about IBD, the microbiome and healthy nutrition. That comic book is also available as a free download in English, Hebrew, French, Spanish and Dutch.
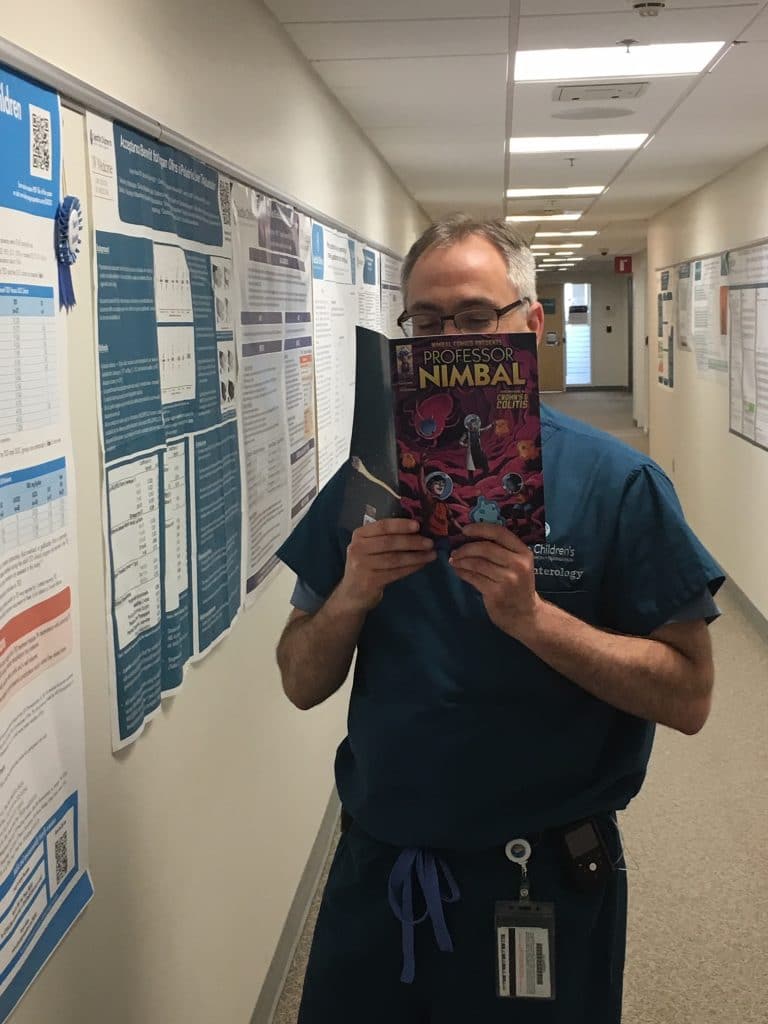
To celebrate the translation of his comic book to multiple languages, Doctor Suskind shared his vision and current insights with us when he agreed to answer questions submitted by IBD parents. Please note that each of the questions can easily be a topic for a doctoral dissertation in itself. Given the interview format and the many topics that parents asked to touch on, his answers had to remain short.
You are a very busy clinical gastroenterologist and research scientist, yet you took time to write the comic book Professor Nimbal. What was your goal with this comic book?
I wanted to make sure that pediatric patients with IBD really understood the what, why and how of IBD and its occurance. It can be hard to convey all that information during a relatively short clinic visit and I thought it would be a fun way to learn about something that is not so fun. My goal with the comic book was to educate and empower patients and their families to take control of their IBD.
You are involved in extensive IBD research. What advances in research are you most excited about? Is there a cure or big break-through coming in the near future?
For many years IBD research focused only on the immune system. Now we know that the microbiome significantly impacts the immune response and that we are able to manipulate it through the foods we eat. This is truly the most exciting aspect of IBD research today. As the research continues and we learn more, I’m confident that we will be able to manipulate the microbiome with more efficacy and make dietary therapy even more personalized.
We already know that any given type of dietary therapy does not work equally well for all patients. With the tools that are currently available to us, what is the best way to personalize diet therapy?
This is a great question. Personalized dietary therapy is truly the end goal. At one point I do believe this will be a reality. Until then, taking a stepwise approach to dietary intervention is key. For some this may mean following a strict SCD for others this may mean following a strict SCD for a prescribed time and then adding in one food at a time in a organized and measured way. Checking laboratory studies before and after adding in a non-SCD food and seeing how the body responds may work best for some patients.
How close are we to adoption of reliable genetic testing that can help tailor a personalized diet for IBD? What can you share about the science of mapping individuals’ immune systems to tailor treatments to them?
We are realistically at least a decade away from using genetic data to help personalize dietary therapy for IBD. With that being said, we are much closer to clearly understanding how diet will change the fecal microbiome. This knowledge from clinical trials is growing every year and over the next 3 to 5 years we are likely to be able to personalize diet based on an individual’s fecal microbiome.
What additional successful alternative healing methods can one IBD patient explore beside medicine and SCD?
Another great question. Our approach to IBD is holistic and looks at an individual as a whole. Focusing on a patient’s overall well-being including psychological support is key to overall success. The only IBD therapies shown to heal the inflammation within the bowels is diet and or medicine.
Why does diet work for some and not others?
Inflammatory bowel disease is a term used to describe two diseases, Crohn’s disease and ulcerative colitism, which have a well understood natural history to them. We know that both are immune related disorders triggered by environmental factors. For any one patient, the immune dysregulation may be different. There are over 260 genes associated with inflammatory bowel disease. Any one patient is likely to have only one of these associated gene abnormalities. In addition, everyone’s environment is unique. Given the complexity of both an individual’s gene and environment not every patient will respond to dietary therapy.
What is the benchmark for knowing whether SCD is working?
There are a number of important benchmarks to look for if the SCD is working. The first is whether a patient is feeling better and their symptoms are improving. The second is that laboratory studies are normalizing, specifically the sedimentation rate C-reactive protein and Calprotectin. The final important benchmark is that there is mucosal healing on endoscopy and colonoscopy.
Knowing there is no “one diet” for everyone, what foods or classes of foods (gluten, lactose, etc.) should someone with IBD definitely avoid?
Diet matters whether you’re on medication therapy or not. Although there is no one diet for everyone, all patients should remove as much as they can of the highly processed foods, foods with food additives such as emulsifiers, and high sugar foods and consume more vegetables and fruits.
This question is about children both on medication and SCD. How long should a child be in remission before medication can be titrated down and only SCD used?
Thanks for asking this question. The answer is that it is dependent on the child and the severity of disease that the patient had prior to receiving therapy. There is a ongoing study that is looking to answer this question specifically. Until then, working with your gastroenterologist to find what will work best for you is the gold standard.
What are the percentile chances of a child “outgrowing” UC when diagnosed at a toddler age and is there anything we can do to boost those odds?
Sadly, we don’t have a clear answer on whether children or adult patients can “outgrow” their disease. It is unlikely that a patient will “outgrow” their disease. Most patients will likely need a therapy whether medication or dietary.
Can children experience gastrointestinal problems, remain undiagnosed with an IBD or IBS (tests are negative) for some time before their symptoms become full blown IBD or IBS? What could prevent full blown IBD?
The simple answer is yes. Inflammation associated with IBD can be present even when a patient has no symptoms. We have no means to prevent IBD however, given the fact that the microbiome is central to the development of IBD and that diet plays a significant role in shaping it, eating a healthy diet with a focus on vegetables and fruits would be a a possible way of mitigating a person’s probability of developing IBD.
What do you know about vagus nerve stimulation for treatment of IBD?
Vagus nerve stimulation is potentially interesting but has not been studied in any significant way in inflammatory bowel disease. There is preliminary data in Rheumatoid Arthritis showing some mild symptom improvement.
I would like to know your thoughts particularly on resistant starch and it’s role?
There are many types of resistant starch, some that are SCD legal and others that are not. The role of resistant starch is important in inflammatory bowel disease as it can shift the fecal microbiome and can have an effect on the colon itself through their metabolites. Understanding how different types of resistant starch impact the intestinal microbiome will be an important part of future research in IBD.
What would you like to see being taught in medical school in regards to autoimmune diseases, IBD, etc. It seems like GI’s don’t have a framework to think about diet and nutrition because they don’t even study it.
Diet is central to medicine. Its effects on the body are seen and accepted within the world of cardiovascular disease, obesity work, celiac disease, allergy issues and in many other medical diseases. We clearly know that it is central in inflammatory bowel disease. The medical community has understood this for many years but have not had the ability to alter medical education until more recently.